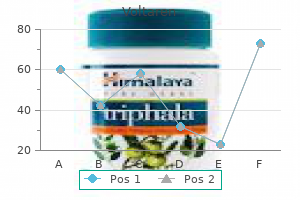
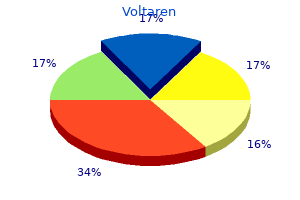
Voltaren
Ana Paola Uranga, MD, MBA
- Department of Emergency Medicine
- University of California, San Francisco-Fresno
- Fresno, California
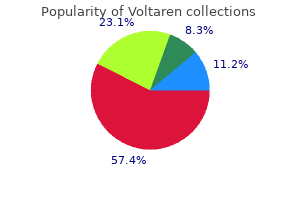
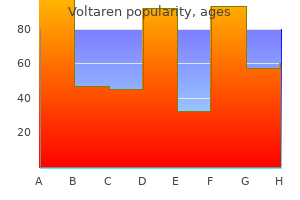
Voltaren dosages: 100 mg, 50 mg
Voltaren packs: 60 pills, 90 pills, 180 pills, 270 pills, 360 pills

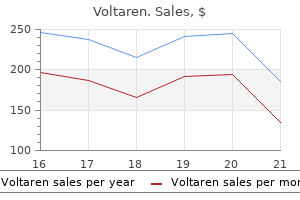
Buy cheap voltaren 50 mg online
The apical suspension should cut back prolapse of the apex in addition to the apical segments of the anterior posterior vaginal wall arthritis in the fingers pictures cheap voltaren 100mg on-line. The apical tail of the graft is sutured to the anterior longitudinal ligament on the stage of S1 with two or three permanent monofilament sutures; alternatively titanium tacks can additionally be used to connect the mesh to the anterior longitudinal ligament sacrum arthritis qualify for disability buy voltaren 100 mg free shipping. These uncommon circumstances have been reported within the literature rheumatoid arthritis awareness order voltaren 50mg without prescription, and most are related to suture or tack placement in the presacral house (Collins et al. Once the graft has been retroperitonealized, cystoscopy is performed to rule out injury to the bladder, intravesical suture, or mesh perforation and to confirm ureteral patency. Significant hemorrhage could occur from disruption of the presacral vessels, and the incidence of this complication may be decreased when fixation of the graft is performed greater on the sacral promontory. Dealing with these vessels preemptively with bipolar vitality, particularly with a minimally invasive approach, might preclude this complication. Vaginal publicity of mesh is one other complication and is heralded by persistent pain, discharge, or infections, and clinicians must be vigilant in follow-up (Karlovsky et al. Symptoms develop on common 14 months after surgery and classically encompass vaginal bleeding and discharge (Kohli et al. Exposures occur more usually with Teflon or Gore-Tex�type materials and are much less frequent with macroporous, monofilament meshes. In sufferers present process a combined operation, supracervical hysterectomy or a meticulous two-layer closure of the cuff ought to be carried out to decrease the incidence of mesh exposure. In patients needing hysterectomy, the feasibility of a supracervical hysterectomy must be strongly examined. Mean operative time was 124 minutes (range 55�185) with a 3% (range 0�11%) conversion fee. Objective remedy was achieved in 91% of sufferers and related satisfaction charges of 92% (Lee et al. Only a few well-designed comparative research exist, and heaps of have varying goal and subjective outcomes. Secondary outcomes included procedure time, quantity of estimated blood loss, hospital keep, perioperative complications, reinterventions, composite end result of success (defined as no prolapse beyond the hymen), no bothersome bulge signs, and no repeat surgical procedure or pessary use for recurrent prolapse within 12 months and long-term complications. In both teams, there have been no recurrences of stage 2 or larger of the apical compartment. Two sufferers in the laparoscopy group had bothersome bulge symptoms in contrast with 4 in abdominal group. In both groups extra members became sexually energetic, there was much less dyspareunia, and the coital frequency was increased at 12 months postoperatively. Secondary outcomes have been intraoperative blood loss, imply drop in hemoglobin, size of postoperative hospitalization, working time, postoperative ache assessment, return to daily actions, QoL, new onset of urinary incontinence, and reoperation charges. At 1 yr, level C met equivalence standards for the belly and laparoscopic groups (6. Secondary outcomes included blood loss, operative time, length of keep, blood transfusion, pulmonary embolus, gastrointestinal or genitourinary tract harm, ileus, bowel obstruction, postoperative fever, pneumonia, wound an infection, and urinary retention. There have been no gastrointestinal tract injuries, and there was one cystotomy in each surgical procedure group (P = 1. Laparoscopic Sacrocolpopexy Versus Robotic-Assisted Sacrocolpopexy Versus Abdominal Sacrocolpopexy (Table 124. Laparoscopic and robotic instances had been analyzed as minimally invasive sacrocolpopexy. Anatomic failures were higher within the open group in contrast with the minimally invasive group (24. Compared with ladies who underwent minimally invasive sacrocolpopexy, girls present process open sacrocolpopexy had a better operative blood loss (188 vs. Chapter 124 Vaginal and Abdominal Reconstructive Surgery for Pelvic Organ Prolapse 2809 longer hospital keep (2. In a comparison of conventional and robotic sacrocolpopexy, robotic circumstances had fewer anatomic failures (5. The primary outcome was whole operative time from incision to closure, however secondary outcomes included postoperative ache, useful activity, bowel and bladder symptoms, QoL, anatomic vaginal help, and price from a well being care perspective. Total operative time was considerably longer within the robotic group (227 +/-47 versus 162 +/-47 min; P < 0. Long-term success and complication information from well-designed studies for sacrocolpopexy are restricted. Follow-up ranged from 1 to 28 months with median (interquartile range) follow-up time for each group: uterosacral colpopexy, 6. The fascinating aspect of this research, nevertheless, was that the authors were capable of extrapolate long-term outcomes. Mean operative time significantly decreased from 196 to 162 min when evaluating the first 15 versus the final 30 circumstances. Mean operative time decreased from 222 min in the course of the first 10 cases to 183 for the next 10 cases. The value of minimally invasive prolapse surgical procedure has been compared with open, vaginal, laparoscopic, and robotic procedures. Surgical costs could be calculated in several different ways; consequently, comparison of price information may be difficult (Tarr and Paraiso, 2015). Vaginal procedures do have excessive success rates with low operation charges and will be the process of alternative for lots of older ladies. The 2016 Cochrane evaluate concluded that there was no evidence of any difference for any of the first outcomes between various sorts of apical vaginal native tissue repairs. In addition, they noted that relating to uterine preservation, sacrospinous hysteropexy was not inferior to vaginal hysterectomy with uterosacral suspension for the treatment of apical uterovaginal prolapse. Colpocleisis Colpocleisis is an obliterative process used in the therapy of post-hysterectomy vaginal vault prolapse or vital uterovaginal prolapse. This process includes creating lateral channels to enable potential uterine drainage. Advantages of the colpocleisis procedures are shorter operative time, ability to use regional anesthesia or native anesthesia with sedation, minimal problems, minimal recurrence, and decreased recuperative time (Cespedes et al. In these whose uterus is to be left in situ, preoperative analysis ought to embrace a Papanicolaou smear, pelvic sonogram, and endometrial biopsy if indicated. Performance of hysterectomy at the time of colpocleisis eliminates the chance of developing cervical or endometrial most cancers and eliminates the danger of growing pyometra, which is a severe complication of partial colpocleisis when the channels become obstructed (Shayya et al. However, most patients chosen for colpocleisis are older with vital comorbidities that make a concomitant hysterectomy undesirable. The cervix is grasped with a tenaculum, and an oblong segment of vaginal epithelium is marked anteriorly and posteriorly. The excision of the vaginal epithelium will prolong 3 cm from the urethral meatus to 3 cm from the cervix (Cespedes et al. It is necessary to depart sufficient vaginal epithelium laterally to permit creation of the lateral channels to facilitate drainage. It is elective to place a 14-Fr Red Robinson catheter or a vessel loop alongside the vaginal sidewalls to help in forming the channels. A excessive perineorrhaphy (levator myorrhaphy) is essential to slender the introitus and stop recurrence.
Buy voltaren 50 mg cheap
Some of the urologic malignancies might progress to some extent the place palliative care is suitable rheumatoid arthritis x-ray appearance best 50mg voltaren. When treatment of the condition is no longer attainable rheumatoid arthritis numbness generic 100mg voltaren amex, treatment can shift to a palliative care mode arthritis in fingers in 20s purchase 100 mg voltaren with amex. Indeed, aggressive symptom management is likely certainly one of the hallmark targets of palliative care for many patients. Important elements of high-quality palliative care embrace ache and symptom administration, realization of non-public targets for the patient and household, and coordination of care (Agar et al. Surgical remedy could play a role in choose cases in which cytoreductive remedy for a big tumor burden, or removal of tumor for intractable bleeding or pain may help to relieve symptoms. Treatment is extremely selective and tailor-made particularly to the wants of each particular person patient. Integrated health care delivery fashions that include suppliers from multiple disciplines is feasible and might help to improve the delivery of care in these circumstances (Bergman et al. Among older adults in assisted living facilities, use of hospice providers has been proven to cut back need for nursing home or other institutional placement (Dobbs et al. This can allow patients to stay dwelling at house as long as attainable and can increase qualityof-life outcomes on this setting. Consultation with trained, dedicated palliative care specialists may be extremely useful in offering necessary take care of older adults near the tip of life. Additional analysis and education on these matters will help enhance our capability to present high-quality look after the older adults whom we serve. Gorina Y, Schappert S, Bercovitz A, et al: Prevalence of incontinence amongst older Americans, Vital Health Stat 3 (36):2014. Abrams P, Cardozo L, Fall M, et al: the standardisation of terminology of lower urinary tract operate: report from the Standardisation Subcommittee of the International Continence Society, Neurourol Urodyn 21:167�178, 2002. Agar M, Currow D, Plummer J, et al: Changes in anticholinergic load from common prescribed medicines in palliative care as death approaches, Palliat Med 23:257�265, 2009. American Geriatrics Society 2015 Beers Criteria Update Expert Panel: American Geriatrics Society 2015 up to date beers criteria for probably inappropriate treatment use in older adults, J Am Geriatr Soc sixty three:2227�2246, 2015. Development and validation of a easy risk model incorporating a chart-derived frailty rating, J Am Coll Surg 219:684�694, 2014. Andel R, Hyer K, Slack A: Risk elements for nursing home placement in older adults with and without dementia, J Aging Health 19:213�228, 2007. Anger J, Saigal C, Madison R, et al: Increasing prices of urinary incontinence amongst female Medicare beneficiaries, J Urol 176:247�251, 2006. Angioli R, Montera R, Plotti F, et al: Success rates, quality of life, and feasibility of sacral nerve stimulation in elderly patients: 1-year follow-up, Int Urogynecol J 24:789�794, 2013. Aybek H, Aybek Z, Abban G, et al: Preventive effects of vitamin E against oxidative harm in aged diabetic rat bladders, Urology 77(2):508, e10�14, 2011. Bal K, Ayik S, Issi Y, et al: Sleep evaluation of patients with nocturia and benign prostatic obstruction, Urology eighty:383�388, 2012. Barrois B, Labalette C, Rousseau P, et al: A nationwide prevalence examine of strain ulcers in French hospital inpatients, J Wound Care 17:373�376, 378�379, 2008. Betschart C, Scheiner D, Maake C, et al: Histomorphological evaluation of the urogenital diaphragm in elderly women: a cadaver research, Int Urogynecol J Pelvic Floor Dysfunct 19:1477�1481, 2008. Chapple C, DuBeau C, Ebinger U, et al: Darifenacin treatment of sufferers > or = 65 years with overactive bladder: results of a randomized, controlled, 12-week trial, Curr Med Res Opin 23(10):2347�2358, 2007. Chesnel C, Charlanes A, Hentzen C, et al: Lower urinary tract signs in aged population with a quantity of sclerosis, Int Neurourol J 22:58�64, 2018. Chughtai B, Sedrakyan A, Isaacs A, et al: Long time period security of sacral nerve modulation in Medicare beneficiaries, Neurourol Urodyn 34:659�663, 2015. Bonnal C, Baune B, Mion M, et al: Bacteriuria in a geriatric hospital: influence of an antibiotic enchancment program, J Am Med Dir Assoc 9:605�609, 2008. Booth J, Hagen S, McClurg D, et al: A feasibility research of transcutaneous posterior tibial nerve stimulation for bladder and bowel dysfunction in elderly adults in residential care, J Am Med Dir Assoc 14:270�274, 2013. Bradway C, Miller E, Heivly A, et al: Continence care for obese nursing house residents, Urol Nurs 30:121�129, 2010. Brittain K, Perry S, Shaw C, et al: Isolated urinary, fecal, and double incontinence: prevalence and degree of soiling in stroke survivors, J Am Geriatr Soc fifty four:1915�1919, 2006. Bylow K, Dale W, Mustian K, et al: Falls and bodily performance deficits in older patients with prostate most cancers undergoing androgen deprivation therapy, Urology seventy two:422�427, 2008. Bynum J, Song Y, Fisher E: Variation in prostate-specific antigen screening in males aged 80 and older in fee-for-service Medicare, J Am Geriatr Soc fifty eight:674�680, 2010. Daneman N, Gruneir A, Newman A, et al: Antibiotic use in long-term care services, J Antimicrob Chemother sixty six:2856�2863, 2011. Report from the 4th International Consultation on Incontinence, Neurourol Urodyn 29(1):165�178, 2010. Prospective ultrastructural/urodynamic evaluation of its natural evolution, J Urol 157:1814�1822, 1997. Endeshaw Y: Correlates of self-reported nocturia amongst community-dwelling older adults, J Gerontol A Biol Sci Med Sci 64:142�148, 2009. Eriksson I, Gustafson Y, Fagerstrom L, et al: Urinary tract infection in very old women is associated with delirium, Int Psychogeriatr 23:496�502, 2011. Ersoz M, Erhan B, Akkoc Y, et al: An analysis of bladder emptying methods and the impact of demographic and scientific factors on spontaneous voiding frequency in stroke patients, Neurol Sci 34:729�734, 2013. Fagan M, Maehlen M, Lindbaek M, et al: Antibiotic prescribing in nursing houses in an space with low prevalence of antibiotic resistance: compliance with national pointers, Scan J Prim Health Care 30:10�15, 2012. Garre-Olmo J, Planas-Pujol X, Lopez-Pousa S, et al: Prevalence and risk factors of suspected elder abuse subtypes in people aged seventy five and older, J Am Geriatr Soc fifty seven:815�822, 2009. Gesenberg A, Sintermann R: Management of benign prostatic hyperplasia in excessive danger sufferers: long-term expertise with the Memotherm stent, J Urol a hundred and sixty:72�76, 1998. Gooren L, Lips P: Conjectures concerning cross-sex hormone remedy of growing older transsexual persons, J Sex Med eleven:2012�2019, 2014. Gotoh M, Matsukawa Y, Yoshikawa Y, et al: Impact of urinary incontinence on the psychological burden of household caregivers, Neurourol Urodyn 28:492�496, 2009. Federal Interagency Forum on Aging-Related Statistics: Older Americans 2012: Key indicators of well-being. Fontana L, Addante F, Copetti M, et al: Identification of a metabolic signature for multidimensional impairment and mortality danger in hospitalized older patients, Aging Cell 12:459�466, 2013. Fox C, Smith T, Maidment I, et al: Effect of medications with anti-cholinergic properties on cognitive function, delirium, physical perform and mortality: a scientific review, Age Ageing 43:604�615, 2014. Fraisse T, Crouzet J, Lachaud L, et al: Candiduria in these over 85 years old: a retrospective research of seventy three sufferers, Intern Med 50:1935�1940, 2011. Frost M, Wraae K, Gudex C, et al: Chronic illnesses in elderly men: underreporting and underdiagnosis, Age Ageing 41:177�183, 2012. Fung C, Pandya C, Guancial E, et al: Impact of bladder most cancers on health related quality of life in 1,476 older Americans: a cross-sectional study, J Urol 192:690�695, 2014. Galizia G, Langellotto A, Cacciatore F, et al: Association between nocturia and falls-related long-term mortality danger in the aged, J Am Med Dir Assoc 13:640�644, 2012. Guillotreau J, Miocinovic R, Game X, et al: Outcomes of laparoscopic and robotic radical cystectomy within the aged sufferers, Urology seventy nine:585�590, 2012. Haruta H, Sakakibara R, Ogata T, et al: Inhibitory control task is decreased in vascular incontinence sufferers, Clin Auton Res 23:85�89, 2013.
Voltaren 100mg cheap
A vaginal ring retractor could also be used to retract the labia majora and arthritis in dogs order voltaren 100 mg otc, later within the case rheumatoid arthritis hand exercises discount voltaren 50mg with amex, to retract the incision arthritis symptoms in dogs front legs cheap voltaren 100mg overnight delivery, additional enhancing visualization and ease of dissection. The knee is elevated and supported with a 1-L bag of intravenous fluid or an acceptable cushion or pad. The involved extremity is internally rotated on the hip and secured to the desk using 3-inch tape, below the operative website. The thigh is prepared and draped to expose its anterolateral facet from the greater trochanter to the patella distally. The higher trochanter and lateral femoral condyle of the femur are identified and marked. These landmarks denote the proximal and distal attachments of the fascia lata (Dwyer and Kreder, 2008). Slings: Autologous, Biologic, Synthetic, and Mid-urethral 2837 Graft Harvest for Autologous Pubovaginal Sling A 6- to 7-cm Pfannenstiel incision is made roughly 2 cm above the pubic symphysis and carried right down to the rectus fascia. A 2-cm � 8-cm graft is then marked out on the rectus fascia in a transverse or longitudinal direction. If a transverse fascial incision is used, maintaining a 2-cm or larger distance away from the pubic symphysis will help ensure a tension-free fascial closure. Freeing the edges of the fascia away from the underlying rectus muscle with a scalpel or electrocautery can also help in a tension-free closure however might theoretically weaken the fascia. Alternatively, figure-of-eight 0-0 polyglactin 910 (Vicryl) could additionally be utilized in women with minimal subcutaneous fat. On a sterile aspect desk, the overlying fat and perifascial tissue are cleaned off the graft and a separate No. Each suture ought to be positioned perpendicular to the sling fibers (transverse harvest only), run throughout every end of the graft, and tied down. Sutures are left long, and the graft is again positioned in the saline solution until wanted. Dissection is carried down to the level of the fascia lata, where two parallel, longitudinal, incisions are made 2 cm aside. The graft is bluntly lifted off the underlying muscle and clamped as far distally as attainable with a right-angle clamp (3 cm to four cm) and transected, permitting one free finish. The fascia lata is separated from both the adipose tissue and muscle fibers by passing the retractor superficially and deep to the fascia lata. With the free distal finish under tension, a Crawford fascial stripper is used to lengthen the fascial incision proximally and divide it earlier than elimination. Classically, a full-length fascial strip (20 cm � 2 cm) was harvested; however, shorter lengths (8 cm) are actually commonly used (Karram and Bhatia, 1990). Immediate compression is utilized to the thigh to constrict any perforating vessels and the area is carefully evaluated for arterial bleeding earlier than closure. The wound is irrigated and closed in three layers without closing the fascia lata. The compressive bandage should stay in place for 8 hours postoperatively and early ambulation must be encouraged (Dwyer and Kreder, 2008). A 15-blade knife is used to carry this incision down through the vaginal epithelium, with care to stay above the periurethral and pubocervical fascia (to avoid bleeding and injury to the urethra and bladder). Alternatively, a midline vaginal incision extending from the bladder base proximally to the mid-urethra distally can be used. With an Allis clamp and Metzenbaum scissors, thick vaginal epithelial flaps are created. It is necessary to maintain the arms of the inverted U-incision extensive to keep away from devascularizing the flap. Once sufficient lateral flaps have been created, the endopelvic fascia ought to now be perforated under the simply palpable ischiopubic rami. Perforation occurs in a superolateral course, and the Metzenbaum scissors are spread extensively to help in the next step of dissection. With this dissection, the infrapubic and retropubic dissection planes are actually related. During this step, it could be very important be certain that the retropubic area is absolutely opened. The posterior floor of the pubic symphysis ought to be easily palpable with little or no intervening tissue. Even though the abdominal fascia is closed, simultaneous finger palpation through the abdominal and vaginal incisions ought to now be potential, while gently palpating the bladder medially. In difficult instances, the most secure dissection airplane into the retropubic house must be instantly adjoining to the periosteum of the pubis, and dissection should be carried out sharply as much as potential to minimize the chance for damage to the pelvic viscera. Pubovaginal Sling Placement and Fixation Stamey or Cobb-Ragde needles are handed from above, via the stomach incision by cautious guidance behind the pubis. Alternatively, bigger surgical instruments similar to tonsil clamps can also be used for suture advancement (Blaivas and Olsson, 1988; McGuire and Lytton, 1978). Again, it is necessary to emphasize that the bladder should be utterly drained earlier than passage of any suture passer to keep away from inadvertent bladder damage. Cystoscopy should be carried out with a 70-degree lens after passage of needles to affirm integrity of the bladder by following the course of needles while an assistant strikes the needles downward and medially towards the bladder. Sagittal view of pubovaginal sling place at bladder neck in retropubic position. To prevent this, it may be very important maintain a distance of two cm or more from the pubic symphysis. In the case of a small bladder harm or inadvertent passage of Stamey needles through the bladder, the needles are removed and handed once more and the procedure is accomplished. Cystoscopy must be carried out after any subsequent needle passage to rule out puncture. After extravesical passage is confirmed, the ureteral orifices are monitored for brisk efflux on each side confirming ureteral patency. Likewise, intravenous methylene blue or sodium fluorescein and ureteral catheters may be used to verify patency. The distal aspect of the graft is sutured to the periurethral tissue with two easy 4-0 Vicryl sutures. After adequate hemostasis is achieved, the vaginal incision is closed with a watertight, running 2-0 Vicryl suture. Before final tensioning of the sling, the vagina must be closed and weighted speculum eliminated to remove distortion that can affect the ultimate rigidity. The Foley catheter is left to straight drainage, and a vaginal packing may be used. Conjugated estrogen cream could also be added to the vaginal packing in postmenopausal girls.
Cheap voltaren 50mg without a prescription
Rohrmann S knee brace for arthritis in the knee voltaren 50mg on line, Katzke V arthritis medication in canada purchase 50 mg voltaren overnight delivery, Kaaks R: Prevalence and development of decrease urinary tract symptoms in an getting older inhabitants arthritis pills for dogs buy 100mg voltaren with mastercard, Urology ninety five:158�163, 2016. Saatli B, Kizildag S, Cagliyan E, et al: Alteration of apoptosis-related genes in postmenopausal women with uterine prolapse, Int Urogynecol J 25:971�977, 2014. Sahin-Onat S, G�zel O, U�ar D: Relationship between urinary incontinence and quality of life/depression in elderly patients, J Clin Gerontol Geriatr 5:86�90, 2014. Sakakibara R, Ito T, Uchiyama T, et al: Lower urinary tract function in dementia of Lewy body kind, J Neurol Neurosurg Psychiatry 76(5):729�732, 2005. Chapter 128 Sicras-Mainar A, Rejas J, Navarro-Artieda R, et al: Antimuscarinic persistence patterns in newly treated patients with overactive bladder: a retrospective comparative analysis, Int Urogynecol J 25:485�492, 2014. Strasser H, Tiefenthaler M, Steinlechner M, et al: Urinary incontinence in the aged and age-dependent apoptosis of rhabdosphincter cells, Lancet 354:918�919, 1999. Strasser H, Tiefenthaler M, Steinlechner M, et al: Age dependent apoptosis and lack of rhabdosphincter cells, J Urol 164:1781�1785, 2000. Sugimoto T, Yoshida M, Ono R, et al: Frontal lobe operate correlates with one-year incidence of urinary incontinence in aged with Alzheimer illness, J Alzheimers Dis 56:567�574, 2017. Suzuki M, Iguchi Y, Igawa Y, et al: Ultrasound-assisted prompted voiding for management of urinary incontinence of nursing residence residents: efficacy and feasibility, Int J Urol 23:786�790, 2016. Tai S, Xu L, Zhang L, et al: Preoperative threat elements of postoperative delirium after transurethral prostatectomy for benign prostatic hyperplasia, Int J Clin Exp Med 8:4569�4574, 2015. Takao T, Tsujimura A, Kiuchi H, et al: Urological surgical procedure in sufferers aged 80 years and older: a 30-year retrospective scientific research, Int J Urol 15:789�793, 2008. Talasz H, Lechleitner M: Polypharmacy and incontinence, Z Gerontol Geriatr 45(6):464�467, 2012. Tani M, Hirayama A, Fujimoto K, et al: Increase in 24-hour urine production/ weight causes nocturnal polyuria as a result of impaired perform of antidiuretic hormone in elderly males, Int J Urol 15:151�154, discussion a hundred and fifty five, 2008. Tannenbaum C, Corcos J, Assalian P: the relationship between sexual exercise and urinary incontinence in older ladies, J Am Geriatr Soc 54:1220�1224, 2006. Tannenbaum C, Drali R, Holroyd-Leduc J, et al: Lessons learned: impression of a continence promotion activity for older community-dwelling girls, Neurourol Urodyn 29:540�544, 2010. Tibaek S, Gard G, Klarskov P, et al: Are exercise limitations associated with decrease urinary tract signs in stroke patients Weatherall M: the risk of hyponatremia in older adults utilizing desmopressin for nocturia: a systematic evaluation and meta-analysis, Neurourol Urodyn 23:302�305, 2004. Wehrberger C, Berger I, Marszalek M, et al: Bladder preservation in octogenarians with invasive bladder cancer, Urology 75:370�375, 2010. Wehrberger C, Jungwirth S, Fischer P, et al: the relationship between cerebral white matter hyperintensities and decrease urinary tract function in a population primarily based, geriatric cohort, Neurourol Urodyn 33:431�436, 2013. Whittle J: How can charges of prostate-specific antigen screening be lowered in males aged eighty and older Tran E, Souhami L, Tanguay S, et al: Bladder conservation treatment within the elderly inhabitants: results and prognostic components of muscle-invasive bladder most cancers, Am J Clin Oncol 32:333�337, 2009. Valente S, DuBeau C, Chancellor D, et al: Epidemiology and demographics of the underactive bladder: a cross-sectional survey, Int Urol Nephrol 46(Suppl 1):S7�S10, 2014. Varli M, Guruz H, Aras S, et al: Asymptomatic bacteriuria among the many aged living in the community: prevalence, risk elements and traits, Eur Geriatr Med 3:87�91, 2012. Vecchioli-Scaldazza C, Morosetti C, Azizi B, et al: Polyacrylamide hydrogel (Bulkamid) in female patients of 80 or more years with urinary incontinence, Int Braz J Urol 40:37�43, 2014. Vethanayagam N, Orrell A, Dahlberg L, et al: Understanding help-seeking in older people with urinary incontinence: an interview examine, Health Soc Care Community 25:1061�1069, 2017. Vij M, Bombieri L, Dua A, et al: Long-term follow-up after colpocleisis: regret, bowel and bladder perform, Int Urogynecol J 25:811�815, 2014. Associations between sexual activity and cognitive operate in older age, Age Ageing forty five:313�317, 2016. Yokoyama O, Yamagami H, Hiro S, et al: Efficacy and security of fesoterodine treatment overactive bladder signs in aged women with and without hypertension, Int J Urol 25:251�257, 2018. Zhang Z, Yang L, Xie D, et al: Depressive signs are discovered to be potential opposed effects of androgen deprivation therapy in older prostate cancer patients: a 15-month potential, observational research, Psychooncology 26:2238�2244, 2017. Zisberg A, Sinoff G, Gur-Yaish N, et al: In-hospital use of continence aids and new-onset urinary incontinence in adults aged 70 and older, J Am Geriatr Soc 59:1099�1104, 2011. Although most fistulae in sufferers within the industrialized world are iatrogenic, they might additionally happen as a result of congenital anomalies, malignancy, inflammation and infection, radiation therapy, iatrogenic (surgical) or external tissue trauma, ischemia, parturition, and a selection of different processes. The continuous leakage of urine and/or fecal materials can have a devastating impact on the standard of lifetime of the patient. Except for a palliative setting, the lively remedy of fistulae is at all times warranted. Although some types of urinary fistulae heal with conservative management, surgical procedure is normally essential for a definitive repair. These must be approached on a case-by-case basis, as a result of restore might involve some progressive and even improvisational maneuvers in the operating room. Ensuring sufficient vitamin is integral to surgical healing in general however is very necessary within the setting of a urinary fistula. Not uncommonly, the catabolic processes contributing to the dearth of healing, which can have been a contributing factor in the initial fistula formation, are often ongoing. This is very relevant in fistulae related to radiation therapy or in debilitated patients. Medicolegal Aspects Acquired urinary fistulae within the industrialized world are almost universally sudden and should end in a great deal of inconvenience, discomfort, and physical disability for the affected individual. They are most frequently acquired as a result of a medical or surgical intervention for an unrelated problem, and, consequently, considerable emotional and psychological misery often accompany the diagnosis and subsequent treatment. Often medicolegal issues occur with a high danger for litigation (Thomas and Williams, 2000). Nevertheless, minimizing patient discomfort, sustaining a positive and sincere patient-physician relationship while providing fixed reassurance, and, lastly, and maybe most important, pursuing expeditious and successful therapy of the fistula most frequently result in a mutually satisfying long-term outcome. Notably, after the preliminary early diagnosis of a urinary fistula, which leads to external urinary leakage, quick management or control of the urinary leakage is important. Addressing this quickly will cut back skin breakdown and associated complications, as nicely as alleviate much of the psychological distress. The judicious use of catheters, pads, skincare, and odor management products and home equipment may be very helpful in this regard. These easy measures can usually deflect the anger of an otherwise very disaffected affected person, thereby reducing the potential for additional aggravating an already tough medical and, presumably, litigious situation. The threat elements for obstructed labor are well known: illiteracy, low financial status, and short stature (<150 cm) (Kasamba et al. The discovering of a persistent fistula after presumably definitive therapy might counsel the existence of different contributing host components, corresponding to malignancy, dietary points, the potential of an unrecognized international physique, tissue ischemia, or surgical components similar to inadequate postoperative urinary drainage, persistent distal urinary obstruction, or technical problems with the surgical procedure (Arrowsmith et al. Preparation and Optimization of Patient Prevention of urinary fistulae is, after all, paramount; nevertheless, nutrition, infection, and malignancy are important issues not only when assessing a patient for the chance of creation of a fistula throughout any given intervention but additionally during an evaluation for the restore of an present urinary fistula. Although the majority of urinary fistulae within the industrialized world occur in wholesome, well-nourished individuals, a nutritional evaluation could also be an important consider some sufferers with fistulae, such as these patients with malignancies. The first surgical repair was described in 1663 by Hendrik von Roonhuyse denuding the fistula margins after which approximating them with sharpened stiff swan quills (Margolis and Mercer, 1994).
Discount voltaren 100mg line
Germain A arthritis nightshades order 50mg voltaren amex, Thibault F arthritis diet and treatment purchase 50mg voltaren visa, Galifet M treating arthritis natural way buy cheap voltaren 100 mg on line, et al: Long-term outcomes after completely robotic sacrocolpopexy for treatment of pelvic organ prolapse, Surg Endosc 27(2):525�529, 2013. Glavind K, Madsen H: A prospective examine of the discrete fascial defect rectocele repair, Acta Obstet Gynecol Scand 79(2):145�147, 2000. Goldman J, Ovadia J, Feldberg D: the Neugebauer-Le Fort operation: a review of 118 partial colpocleises, Eur J Obstet Gynecol Reprod Biol 12(1):31�35, 1981. Good Meadow M, Abele Travis A, Balgobin Sunil, et al: Vascular and ureteral anatomy relative to the midsacral promontory, Am J Obstet Gynecol 208(6):486. Granese R, Candiani M, Perino A, et al: Laparoscopic sacrocolpopexy within the treatment of vaginal vault prolapse: eight years expertise, Eur J Obstet Gynecol Reprod Biol 146(2):227�231, 2009. Kafy Souzan, Huang Jack Y J, Al-Sunaidi Mohammed, et al: Audit of morbidity and mortality rates of 1792 hysterectomies, J Minim Invasive Gynecol 13(1):55�59, 2006. Kapoor Shveta, Sivanesan Kanapathippillai, Robertson Jessica Amy, et al: Sacrospinous hysteropexy: review and meta-analysis of outcomes, Int Urogynecol J 28(9):1285�1294, 2017. Karram M, Goldwasser S, Kleeman S, et al: High uterosacral vaginal vault suspension with fascial reconstruction for vaginal repair of enterocele and vaginal vault prolapse, Am J Obstet Gynecol 185(6):1339�1343, 2001. Karram Mickey, Maher Christopher: Surgery for posterior vaginal wall prolapse, Int Urogynecol J 24(11):1835�1841, 2013. Katrikh Aaron Z, Ettarh Rajuno, Kahn Margie A: Cadaveric nerve and artery proximity to sacrospinous ligament fixation sutures positioned by a suturecapturing gadget, Obstet Gynecol 130(5):1033�1038, 2017. Kenton K, Shott S, Brubaker L: Outcome after rectovaginal fascia reattachment for rectocele restore, Am J Obstet Gynecol 181(6):1360�1363, dialogue 1363�1364, 1999. Kenton Kimberly, Pham Thythy, Mueller Elizabeth, et al: Patient preparedness: an important predictor of surgical outcome, Am J Obstet Gynecol 197(6):654. Kobashi Kathleen C, Leach Gary E, Frederick Robert, et al: Initial expertise with rectocele repair using nonfrozen cadaveric fascia lata interposition, Urology 66(6):1203�1278, 2005. Korbly Nicole B, Kassis Nadine C, Good Meadow M, et al: Patient preferences for uterine preservation and hysterectomy in girls with pelvic organ prolapse, Am J Obstet Gynecol 209(5):470. Gustilo-Ashby A Marcus, Paraiso Marie Fidela R, Jelovsek John Eric, et al: Bowel signs 1 yr after surgery for prolapse: further evaluation of a randomized trial of rectocele repair, Am J Obstet Gynecol 197(1): seventy six. Haessler Alexandra L, Lin Lawrence L, Ho Mat H, et al: Reevaluating occult incontinence, Curr Opin Obstet Gynecol 17(5):535�540, 2005. Hiltunen Reijo, Nieminen Kari, Takala Teuvo, et al: Low-weight polypropylene mesh for anterior vaginal wall prolapse, Obstet Gynecol 110(Suppl):455�462, 2007. Hosni Mohamed M, El-Feky Alaa E H, Agur Wael I, et al: Evaluation of three totally different surgical approaches in repairing paravaginal assist defects: a comparative trial, Arch Gynecol Obstet 288(6):1341�1348, 2013. Hviid Ulla, Hviid Thomas Vauvert F, Rudnicki Martin: Porcine pores and skin collagen implants for anterior vaginal wall prolapse: a randomised prospective controlled examine, Int Urogynecol J 21(5):529�534, 2010. Hyakutake Momoe Tina, Cundiff Geoffrey William, Geoffrion Roxana: Cervical elongation following sacrospinous hysteropexy: a case sequence, Int Urogynecol J 25(6):851�854, 2014. Imparato E, Aspesi G, Rovetta E, et al: Surgical administration and prevention of vaginal vault prolapse, Surg Gynecol Obstet 175(3):233�237, 1992. Iyer Shilpa, Seitz Miriam, Tran Alexis, et al: Anterior colporrhaphy with and with out dermal allograft: a randomized control trial with long-term followup, Female Pelvic Med Reconstr Surg 2018. Krause Hannah G, Goh Judith T W, Sloane Kate, et al: Laparoscopic sacral suture hysteropexy for uterine prolapse, Int Urogynecol J 17(4):378�381, 2006. Kulkarni Mamta Muralidhar, Rogers Rebecca Glenn: Vaginal hysterectomy for benign illness without prolapse, Clin Obstet Gynecol 53(1):5�16, 2010. Lantzsch T, Goepel C, Wolters M, et al: Sacrospinous ligament fixation for vaginal vault prolapse, Arch Gynecol Obstet 265(1):21�25, 2001. Lee Ted, Rosenblum Nirit, Nitti Victor, et al: Uterine sparing robotic-assisted laparoscopic sacrohysteropexy for pelvic organ prolapse: security and feasibility, J Endourol 27(9):1131�1136, 2013. Lowenstein Lior, Fitz Amelia, Kenton Kimberly, et al: Transabdominal uterosacral suspension: outcomes and problems, Am J Obstet Gynecol 200(6):656. Maher Christopher, Baessler Kaven: Surgical administration of posterior vaginal wall prolapse: an evidence-based literature review, Int Urogynecol J 17(1):84�88, 2006a. Maher C, Baessler K: Surgical management of anterior vaginal wall prolapse: an evidence-based literature evaluate, Int Urogynecol J 17(2):195�201, 2006b. Maher Christopher F, Qatawneh Aymen M, Baessler Kaven, et al: Midline rectovaginal fascial plication for restore of rectocele and obstructed defecation, Obstet Gynecol 104(4):685�689, 2004b. Maldonado Pedro A, Stuparich Mallory A, McIntire Donald D, et al: Proximity of uterosacral ligament suspension sutures and S3 sacral nerve to pelvic landmarks, Int Urogynecol J 28(1):77�84, 2017. Margulies Rebecca U, Rogers Mary A M, Morgan Daniel M: Outcomes of transvaginal uterosacral ligament suspension: systematic evaluate and metaanalysis, Am J Obstet Gynecol 202(2):124�134, 2010. Meschia M, Bruschi F, Amicarelli F, et al: the sacrospinous vaginal vault suspension: important analysis of outcomes, Int Urogynecol J Pelvic Floor Dysfunct 10(3):155�159, 1999. Meschia Michele, Pifarotti Paola, Bernasconi Francesco, et al: Porcine skin collagen implants to forestall anterior vaginal wall prolapse recurrence: a multicenter, randomized examine, J Urol 177(1):192�195, 2007. Migliari Roberto, De Angelis Michele, Madeddu Giuliana, et al: Tension-free vaginal mesh repair for anterior vaginal wall prolapse, Eur Urol 38(2):151� a hundred and fifty five, 2000. Novara Giacomo, Artibani Walter: Surgery for pelvic organ prolapse: present status and future perspectives, Curr Opin Urol 15(4):256�262, 2005. Nygaard Ingrid E, McCreery Rebecca, et al: Abdominal sacrocolpopexy: a comprehensive review, Obstet Gynecol 104(4):805�823, 2004b. Olsen A, Smith V, Bergstrom J, et al: Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence, Obstet Gynecol 89(4):501� 506, 1997. Paek Jiheum, Lee Maria, Kim Bo Wook, et al: Robotic or laparoscopic sacrohysteropexy versus open sacrohysteropexy for uterus preservation in pelvic organ prolapse, Int Urogynecol J 27(4):593�599, 2016. Eric, Frick Anna, et al: Laparoscopic in contrast with robotic sacrocolpopexy for vaginal prolapse, Obstet Gynecol 118(5):1005�1013, 2011. Paraiso Marie Fidela R, Barber Matthew D, Muir Tristi W, et al: Rectocele repair: a randomized trial of three surgical methods including graft augmentation, Am J Obstet Gynecol 195(6):1762�1771, 2006. Penalver Manuel, Mekki Yasir, Lafferty Heather, et al: Should sacrospinous ligament fixation for the management of pelvic support defects be part of a residency program process Moiety Fady M Shawky, Hegab Hassan Mansour, Ghanem Ibrahim Abdel Latif, et al: Abdominal sacrohysteropexy for uterovaginal prolapse: a potential examine on 33 cases, Arch Gynecol Obstet 281(4):631�636, 2010. Moreno Sierra Jes�s, Oshiro Elena Ortiz, P�rez Cristina Fernandez, et al: Long-term outcomes after robotic sacrocolpopexy in pelvic organ prolapse: prospective evaluation, Urol Int 86(4):414�418, 2011. Mustafa Susana, Amit Amnon, Filmar Shlomo, et al: Implementation of laparoscopic sacrocolpopexy: establishment of a studying curve and shortterm outcomes, Arch Gynecol Obstet 286(4):983�988, 2012. Natale F, La Penna C, Padoa A, et al: A prospective, randomized, controlled study comparing gynemesh, a synthetic mesh, and pelvicol, a biologic graft, in the surgical treatment of recurrent cystocele, Int Urogynecol J Pelvic Floor Dysfunct 20(1):75�81, 2009. Nicita G: A new operation for genitourinary prolapse, J Urol 160(3 Pt 1):741�745, 1998. Nieminen Kari, Hiltunen Kari-Matti, Laitinen Jukka, et al: Transanal or vaginal approach to rectocele restore: a potential, randomized pilot study, Dis Colon Rectum 47(10):1636�1642, 2004.
Cheap voltaren 100mg without prescription
If an artificial prosthesis or xenograft is being used arthritis knee numbness effective 50mg voltaren, surgeons should thoroughly counsel their patients about the everlasting nature of those merchandise and the unique and generally serious problems associated to their use arthritis in neck at 30 discount voltaren 100mg on-line. In our opinion arthritis in feet images order 50mg voltaren amex, this step is paramount because many sufferers and their households have elevated awareness of the potential risks of artificial mesh. Women also needs to be counseled concerning the threat for transient and permanent voiding dysfunction after surgery. Chapter 125 neuropathic symptoms occurred in all but one lady at a median time to symptom resolution of 31. The stomach (from the umbilicus down) and vagina are ready and draped in sterile style. A weighted speculum is placed within the vagina, and an 18-Fr Foley catheter is inserted into the urethra. The affected person must be positioned in a reasonable Trendelenburg place; for optimum visualization during vaginal dissection, the surgeon may benefit from a headlight. The earliest sequence included a diverse and complicated affected person population, including women with pelvic radiation, diabetes, spinal cord injury, and pelvic trauma (Blaivas and Jacobs, 1991; McGuire et al. Several notable modifications have been described over the years that confirm the flexibility of this system. However, by 6 months, these symptoms had resolved in all but three girls (5%), who remained on anticholinergic treatment. In their research, 92% of the 36 cystoceles were thought-about cured at a median of 20 months after surgical procedure. While Pubovaginal Sling Postoperative Care the patient is allowed liberal fluids and food regimen the night of surgical procedure and the vaginal packing and urethral catheter are each removed on the morning of the primary postoperative day. Patients are instructed to keep away from lifting in extra of 10 pounds and sexual intercourse for a minimum of 6 weeks after surgery. Sexual intercourse ought to be resumed only after a physical examination and affirmation of vaginal therapeutic by the surgeon. The latter examine assessed outcomes utilizing a quality-of-life (QoL) questionnaire and located the success rate to be lower (81%). Postoperative problems included a pelvic abscess related to a prior cadaveric sling, pubic osteomyelitis related to a prior bone-anchored sling, and one case of long-term urinary retention. The authors retrospectively assessed outcomes utilizing four totally different validated questionnaires and found that 72% of ladies had been continent and only 3. The disparity between subjective patient outcomes and strict goal remedy is another important statement, indicating that postoperative satisfaction is possible even in absence of complete dryness. The authors reported an 85% overall success rate (markedly improved or cured incontinence) and a history of previous anti-incontinence surgery had no effect on success charges. At a median followup of 89 months, 63% of eighty four women had been improved or cured per validated questionnaire. It is attention-grabbing to observe that the authors tested intraoperative urethral stress to make sure that the slings might create pressures of 80 to 90 cm H2O. This affected person satisfaction�derived cure fee was similar to the questionnaire-based outcomes noted by Brown and Govier (2000). All of the women in this study had thigh ache at 1 to 2 weeks, and 11% described persistent thigh pain at 6 weeks. Despite this, 83% of respondents indicated that the procedure had a constructive effect on their life, 82% would advocate the surgery to a friend, and 83% would undergo the process again. Postoperative de novo or urgency incontinence charges range from 2% to 22% (Albo et al. In general, the outcome data are restricted, and the efficacy and sturdiness of those slings are questionable. Experience has shown that these tissue-processing strategies can have deleterious results on cadaveric sling outcomes (Nazemi et al. Several groups have commented on the standing of cadaveric tissues at reoperation for sling failure. Histopathologic analyses of the retrieved materials indicated the next ongoing processes within the failed graft: disorganized transforming, areas of graft degeneration, and proof of immune reaction. Since then, further groups have documented high failure charges with freeze-dried allografts. The average time to reoperation was 9 months (range 3 to 15), and intraoperative findings at reoperation revealed the entire allograft to be fragmented, attenuated, or simply absent. Seven of the eight ladies had a number of comorbidities, together with neurologic illness, diabetes, previous pelvic irradiation, and former anti-incontinence and pelvic surgery. Histologic examination of the retrieved allograft revealed wavy collagen fibers with loosely packed fibroblasts and focal areas of degeneration. However, at intermediate follow-up, only 32% of the women were dry, and 36% noted improvement. Surgical re-exploration revealed virtually complete absence of graft material, without proof of infection or extreme inflammatory response. Four groups discovered the outcomes comparable with similarly high success charges and no negligible distinction in problems. With long-term follow-up, two groups noted superior continence outcomes in the autologous group (Almeida et al. Some research assist the efficacy of solvent-dehydrated fascial slings (Frederick and Leach, 2005; Nazemi et al. Seventeen girls had been randomized to sling, and the authors concluded that the artificial suburethral sling had equivalent outcomes to the modified Burch process after 3 months of follow-up. It is fascinating to observe that, although the authors reported no issues with exposure or perforation, they state in their discussion section that they stopped utilizing this type of sling because of issues reported in 1995 by Weinberger and Ostergard. Forty p.c developed a wound complication and 21% required full or partial sling removal (10 with sinus tract formation, 4 with persistent vaginal granulation, three with prosthetic exposure, and 1 with groin pain). Likewise, there have additionally been issues with different artificial sling supplies (polyethylene and polypropylene) with less-than-ideal bodily properties placed underneath rigidity at the bladder neck (Drutz et al. In general, xenografts are associated with a low rate of an infection, exposure, and perforation due to their incorporation into host tissue (Rutner et al. The majority of studies in the literature report on gamma-sterilized, porcine dermis (Pelvicol, C. Evidence of a significant immunologic or persistent inflammatory reaction was absent. These authors concluded that the advanced incorporation of the implant would lend to good biocompatibility. There was no statistical distinction with regard to complication rates or postoperative pad rating. Tissue breakdown, represented by intermittent areas of myxoid degeneration, was present and may have indicated evidence of early graft failure. However, anti-incontinence surgery may treatment, improve, or irritate storage signs. This aspect of anti-incontinence surgery is unpredictable and a major reason for affected person dissatisfaction. Although 97% of the women were continent, only 78% were happy with the surgical end result because of persistent or de novo urgency symptoms. The storage symptoms ultimately resolved in 69% of the ladies, virtually all of whom had a closed bladder neck at relaxation.
Cheap voltaren 50 mg otc
Alternatively arthritis itchy fingers cheap voltaren 100 mg otc, if an aggressive posterior vaginal dissection to the perineum is to be performed (see later) for placement of an prolonged piece of posterior mesh with subsequent retroperitonealization of the mesh rheumatoid arthritis doctors cheap 50 mg voltaren amex, the culdoplasty is often not needed arthritis hip diet quality 50mg voltaren. Some pelvic surgeons perform minimal dissection of the peritoneum and bladder off the vagina, sufficient to fix the mesh for four to 5 cm on all sides, whereas different methods describe a more in depth dissection that entails lifting the posterior bladder wall and trigone off the underlying vagina, in addition to dissecting all the best way to the perineal physique. Care is taken to establish the border of the bladder to avoid suturing the graft to the bladder and to secure the lateralmost portions of the mesh to forestall folding. An obturator in the vagina is useful to facilitate suture placement and safe the mesh to the vagina. The graft is secured to the vagina by folding over the cuff of the vagina and permitting the lengthy finish of the graft to exit posteriorly and prolong to the sacrum. The quick arm of the this positioned on the top of the vagina, and the lengthy arm of the this secured to the decrease finish of the vagina. The posterior section of the mesh is then hooked up to the posterior vaginal wall with 6 to 8 interrupted monofilament delayed absorbable or nonabsorbable sutures. At this step, the central sutures from the culdoplasty are placed through the lengthy arm of the mesh if desired. Placing the obturator all the method in which into the vagina however not pushing the vagina upward establishes the correct size for the graft. The graft is placed along the best lateral side of the rectum within the area beforehand developed by extending the opening of the peritoneum from the sacrum. With this technique, the vaginal vault is connected to the fascia of the iliococcygeus muscle as the anchoring web site in distinction to the uterosacral or sacrospinous ligaments. The fascia of the iliococcygeus muscle is identified lateral to the rectum and distal the ischial spine (Shull et al. It is recommended that bilateral suture fixation be performed to achieve optimum outcomes. Special needle drivers and lighted retraction are helpful to facilitate suture placement. In circumstances using everlasting suture a pulley-stitch approach is utilized, tying the knot internally. Eight sufferers skilled pelvic help loss postoperatively, three in the middle (apical) compartment, 2 within the posterior compartment, and 4 within the anterior compartment. Intraoperative complications included rectal and bladder laceration and hemorrhage requiring transfusion. Postoperative problems included vaginal cuff abscess, fever, and transient femoral neuropathy. As mentioned earlier, other pelvic floor defects and stress urinary incontinence can be addressed at the identical time. In addition to open surgery, robotic-assisted laparoscopic and pure laparoscopic approaches have been described and are commonly used right now (Daneshgari et al. The critical components of the operation embrace the use of permanent mesh (polypropylene) or autologous fascia as graft materials and safe fixation of the graft to the sacral promontory and vaginal cuff. The patient is positioned within the low lithotomy place, offering transvaginal and transabdominal access. Upon surgical entry into the peritoneal cavity, it may be very important achieve exposure of true pelvis by cautious packing of the small gut and sigmoid colon. This is accomplished by releasing all adhesions within the pelvis and packing the bowel above the extent of the sacral promontory and displacing the sigmoid to the left, exposing the sacral promontory and posterior peritoneum. An incision is made in the posterior peritoneum over the sacral promontory, extending inferiorly alongside the right lateral side of the rectum in the course of the cul-de-sac. Electrocautery is used when dividing the fatty tissue over the promontory to minimize bleeding and improve visualization. Abdominal sacrocolpopexy Synthetic graft materials is sutured securely to vaginal cuff using a number of interrupted permanent sutures. The peritoneal cul-de-sac is closed using linearly placed sutures to obliterate this potential house. It requires a visible cue of the mesh attachment while extending the vagina cephalad with an end-to-end anastomotic sizer to its maximal length without actively stretching it. Last, the graft is positioned in the retroperitoneal space by closing the posterior peritoneum over the graft and covering the graft on the vagina with the superior fringe of the anterior peritoneum and bladder flap. The affected person is then examined to determine if any ancillary transvaginal prolapse repairs are wanted. Sacrocolpopexy could also be performed with a minimally invasive method using laparoscopy or robotic surgical procedure. The basic steps of the procedure are the identical whether performed abdominally, robotically, or laparoscopically and differ mainly by the method of abdominal entry, trocar placement, docking the robotic patient cart, and technique of suture fixation. After administration of basic anesthesia, the patient is correctly positioned in Allen stirrups in a low lithotomy place, the arms are properly tucked to the aspect, and all bony prominences are padded. A pelvic exam is performed, the stomach and vagina are surgically prepared, a Foley catheter is inserted into the bladder, and nasal/ oral gastric tube is placed. Laparoscopic entry could be carried out with an open or closed method; though the umbilicus is the most frequent site of entry, other sites include the left higher quadrant or subxiphoid and less commonly, transuterine and transvaginal. Typically beginning at the umbilicus, the surgeon makes an incision on the base of the umbilicus and an eight. B, From Scarpero H, Cespedes R, Winters J: Abdominal strategy to the repair of vaginal vault prolapse. The typical robotic instruments used are the robotic monopolar scissors, robotic Maryland bipolar instrument, and a robotic bowel grasper. After any essential adhesiolysis, the bowel is gently swept out of the pelvis and above the pelvic brim. Next the ureters are recognized along the pelvic aspect walls, particularly the best ureter, which is close to the area of dissection. Careful dissection in this area is important to avoid shearing of presacral veins as a end result of severe bleeding might occur. The middle sacral vessel traverses over the promontory and should also be averted. The peritoneum incision is extended alongside the best pelvic side wall into the Douglas cu-de-sac. The upper vagina and vaginal apex should be elevated and distended with a vaginal stent. This permits enough dissection and visualization of the fibromuscular layers of the vaginal wall and aids in graft placement. The vagina is elevated by way of the vaginal stent, and the peritoneum covering the vagina is incised transversely. Dissection should progress simply above the fibromuscular layer within the unfastened areolar tissue of the vaginal wall. Dissecting within the applicable plane decreases the risk of unintended entry into the vagina. Unintentional entry into the vaginal lumen increases the risk of future graft publicity particularly when using artificial mesh. If the vaginal wall is opened, it must be irrigated copiously followed by a two-layer closure with 2-0 or 3-0 delayed absorbable suture.
References
- Diaz EM, Holsinger FC, Zuniga ER, et al. Squamous cell carcinoma of the buccal mucosa: one institution's experience with 119 previously untreated patients. Head Neck 2003;25: 267-273.
- The American Society of Anesthesiologists Task Force on Perioperative Management of Patients with Cardiac Implantable Electronic Devices presents a Practice Advisory for the Perioperative Management of Patients with Cardiac Implantable Electronic Devices: Pacemakers and Implantable Cardioverter- Defibrillators. Anesthesiology. 2011;114:247-61.
- Wagner JD, Mosby EL. Assessment of Proplast-Teflon disc replacements. J. Oral Maxillofac. Surg. 1990;48:1140.
- Cox GB, Fimmel AL, Gibson F, Hatch L. The mechanism of ATP synthase: a reassessment of the function of the a and b subunits. Biochim Biophys Acta 1986;849:62.